Topical Steroids
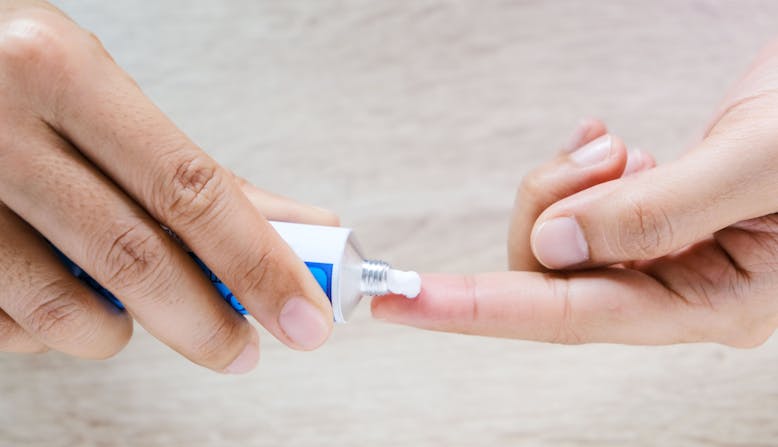
Topical steroids are one of the most common topical treatments for psoriasis. They are derived from the natural corticosteroid hormones produced by the adrenal glands. Corticosteroids control inflammatory responses in the body, among other important functions, making them an ideal anti-inflammatory agent to reduce swelling and redness/discoloration caused by lesions.
Steroids come in various strengths, ranging from very strong or “super-potent” to very weak or “least potent.” You can learn more about potency classification and which steroids fit each classification by looking at the National Psoriasis Foundation’s Topical Steroid Potency Chart.