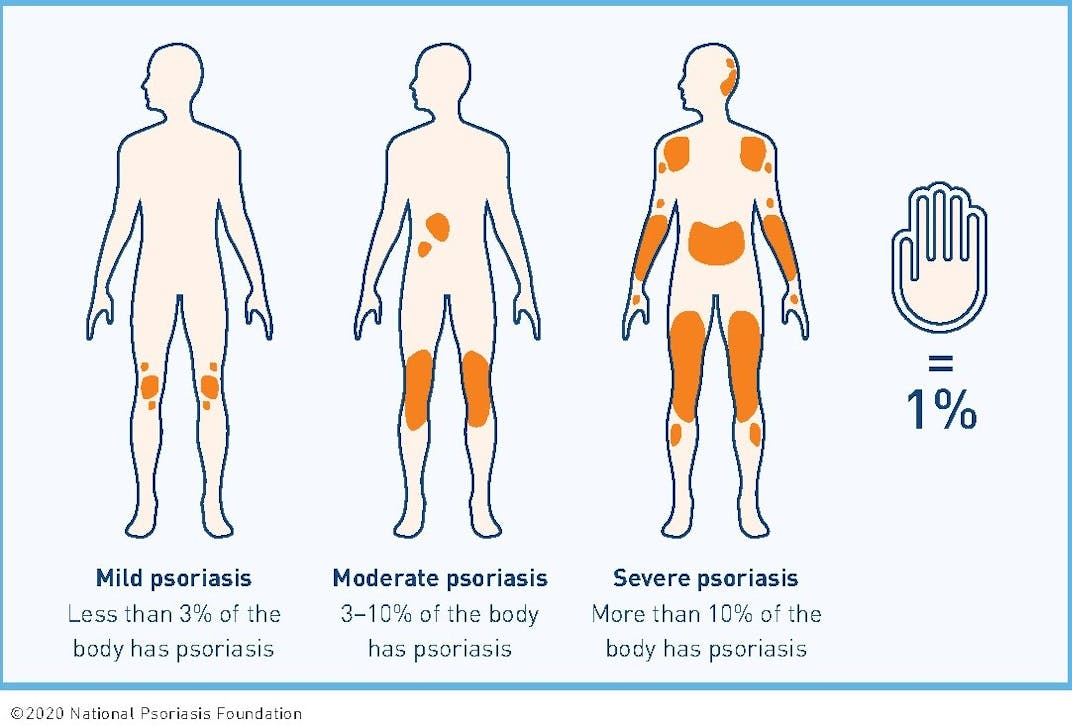
We now know that skin affected by psoriasis is a sign of inflammation occurring in the body. Even people living with mild psoriasis (appearing on less than 3% of the body) may have significant inflammation in the body. Evidence shows that people with mild, moderate or severe psoriasis may also experience psoriatic arthritis and other comorbidities.
Why Treat?
Psoriasis is not just a skin disease.
Although doctors and patients thought it was simply a skin disease decades ago, science has since advanced our understanding of psoriasis and how it affects the whole body.

That is why treating psoriasis is so important. Effective treatment of your psoriasis not only manages skin symptoms but may also help to reduce inflammation in your body that could lead to other diseases. These other diseases are often referred to as comorbidities.
A comorbidity is a disease or condition that occurs because of or is related to a health condition you have, such as psoriasis. Common comorbidities of psoriasis include psoriatic arthritis, cardiovascular (heart) disease, metabolic syndrome and mental health concerns.
Learn more by requesting a free comorbidites quick guide.
There may be other reasons that you choose to treat your psoriasis. You may want to manage the intense itch and pain affecting your skin. You may want to feel confident wearing certain clothes. You may be tired of brushing off or vacuuming scales that fall from plaques. You may long to talk with people and know they are listening to you and not staring at your plaques. These are all valid reasons to treat your psoriasis.
Whatever your motivation for treating, know that there are more options available now than ever before. Discuss with your dermatologist ways to effectively treat your psoriasis.
If you are not seeing an improvement in your symptoms after three to six months, discuss with your dermatologist other treatment options or changes to your current treatment. Your dermatologist should take a treat to target approach. Under Treat to Target, a patient and their health care provider set specific targets or goals for improved health outcomes. The goals are meant to reduce the severity of plaque psoriasis so that it covers 1 percent or less of a person's body within three months after starting a treatment. Since your treatment may also affect your overall health, continue to see your primary care provider for regular check-ups.
Contact the Patient Navigation Center
Learn more about psoriasis and treatment options.